The Cervical Cancer Guide: Knowledge is Prevention
- Medfix

- 18 hours ago
- 6 min read

At Medfix, we believe health information should be direct. You do not need a medical degree to understand your risks or your options. Here is the breakdown of how this cancer works and how it is treated.
Cervical cancer is the 4th most common cancer in women globally. It is also one of the most preventable.
It happens in the cervix, which is the neck of the womb that connects to the vagina.

How it Stars: HPV
In fact, 99% of cervical cancer cases are caused by the Human Papillomavirus.
If you are sexually active, you will likely get HPV. Most of the time, your immune system kills it off, and you never even know you had it. The problem starts when the infection becomes persistent. When certain high-risk strains of HPV hang around for years, they start to rewrite the DNA of your cervical cells. If those changes are not caught, they eventually turn into cancer.

Risk Factors Beyond the Virus
While HPV is the main trigger, other factors make it easier for the cancer to take hold.
Smoking: Tobacco byproducts damage cervical cell DNA and weaken the immune response in the cervical tissue.
Long-term Oral Contraceptives: Using birth control pills for more than 5 years is linked to a higher risk, though this often balances out once you stop taking them.
Immune Suppression: Conditions like HIV or even chronic high stress and poor nutrition make it harder for your body to fight off the virus.
Pregnancy History: Having 3 or more full-term pregnancies is associated with an increased risk.
Family History: If your mother or sister had cervical cancer, your chances are slightly higher.
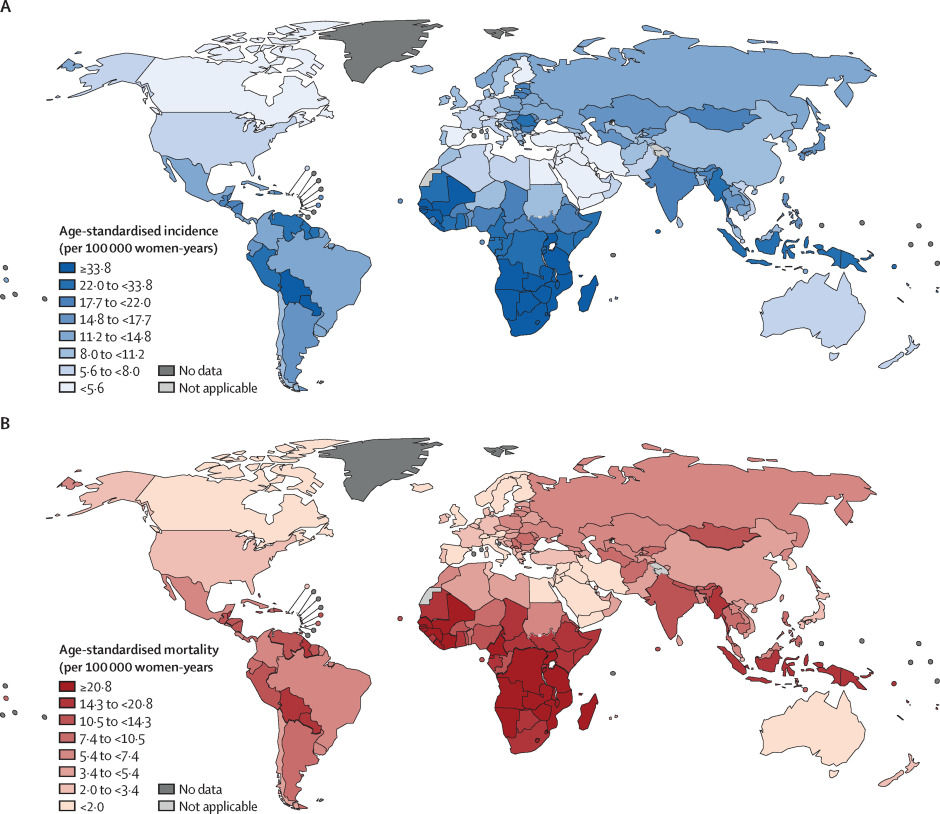
The Statistics
Understanding the scale of this disease helps clarify why screening is so important.
Globally: Over 600,000 women are diagnosed with invasive cervical cancer every year. Tragically, approximately 350,000 women worldwide die from the disease annually.
In the United States: The American Cancer Society estimates about 13,000 new cases annually. More than 4,000 women in the U.S. die from the disease each year. While these numbers are still too high, the U.S. has a much better handle on the disease than many other countries. This is largely due to widespread access to routine screenings and advanced medical care, which have significantly lowered both the number of cases and the death rate over the last few decades.
The Power of Early Detection: The timing of the diagnosis changes everything:
Early Detection: If caught early, the 5-year survival rate is over 90%.
Late Detection: If the cancer is found after it has spread to distant organs, the survival rate drops to around 19%.
These figures prove that regular screening is the most effective way to stay on the right side of these numbers.

Symptoms: Why You Cannot Wait for Them
In the early stages, cervical cancer is silent. You will not feel it. By the time symptoms appear, the cancer has usually started to invade deeper tissue. This is why waiting for "signs" is dangerous; the goal is to find changes before they ever become symptomatic.
Signs that require a doctor visit include:
Abnormal Bleeding: This is the most common sign. It includes bleeding after sex, bleeding between regular periods, or any bleeding after you have already gone through menopause.
Changes in Discharge: Watch for vaginal discharge that is watery, bloody, or has a persistent foul odor.
Pain During Intercourse: Feeling pain or discomfort during sex is not normal and should be checked.
Pelvic or Back Pain: Persistent pain in the pelvic region or lower back that isn't related to your period or other known activity.
Advanced Symptoms: As the disease progresses, it can cause more severe issues such as:
Leg swelling (usually in one leg).
Difficulty or pain when peeing or having bowel movements.
Blood in the urine.
Unexplained weight loss or constant fatigue.
If you experience any of these, don't panic. Many of these symptoms can be caused by other, less serious issues. However, you should see a doctor right away to be sure.

The Diagnostic Path
If a screening comes back abnormal, it does not mean you have cancer. It usually just means your doctor needs to take a closer look. Here is the process, starting with the initial test:
Pap Smear: This is the first step. A doctor takes a small sample of cells from the surface of your cervix to check for any changes under a microscope.
Colposcopy: If the Pap smear shows something unusual, the doctor uses a special magnifying tool to look closely at the cervix. They may use a vinegar-like solution to make abnormal areas easier to see.
Biopsy: During a colposcopy, the doctor might take a tiny piece of tissue. This is the only way to be 100% sure if the cells are cancerous or just pre-cancerous.
LEEP (Loop Electrosurgical Excision Procedure): This uses a thin wire loop with an electric current to remove a larger section of tissue. It’s helpful because it can act as a more detailed test and a treatment at the same time by removing the abnormal cells.

Treatment and Stages
Cervical cancer is graded on a scale from 0 to 4. Your treatment plan depends entirely on how far the cells have traveled from where they started.
Stage 0 (Pre-cancer): These are called "squamous intraepithelial lesions." This means there are abnormal cells, but they aren't cancer yet.
Treatment: Doctors usually remove the area using a LEEP, laser treatment, or cryosurgery (freezing the cells).
Stages 1 & 2 (Early Stage): The cancer is mostly confined to the cervix or the area immediately around it.
Treatment: Surgery is the main tool here. This might be a "cone biopsy" (removing a wedge of the cervix) or a "hysterectomy" (removing the uterus).
Stage 3 (Advanced Stage): The cancer has spread further into nearby tissues or lymph nodes in the pelvis.
Treatment: Doctors typically use a combination of chemotherapy and radiation to target a wider area.
Stage 4 (Metastatic): The cancer has traveled to distant organs, like the lungs or liver.
Treatment: The focus shifts to immunotherapy and palliative care, which focuses on managing symptoms and improving quality of life.

Recovery and Post-Treatment Life
Recovery looks different for everyone depending on the type of treatment. It’s about giving your body time to heal and staying on top of your follow-up care.
Understanding the Recovery Process:
Minor Procedures (LEEP/Cone Biopsy): You might have some light cramping or spotting for a few weeks, but most people return to their routine within a few days.
Surgery (Hysterectomy): This is a major operation. Your body needs several weeks to heal, and you may experience the start of menopause or changes in sexual health.
Radiation Therapy: The effects of radiation happen slowly. It can cause long-term tiredness and changes to the skin and tissues in the pelvic area.
Chemotherapy: Recovery from chemo is focused on regaining your energy and rebuilding your immune system. It can cause temporary hair loss, nausea, and fatigue.
The Monitoring Plan:
First 2 Years: You will have follow-up exams every 3 to 6 months.
After 2 Years: Exams usually move to every 6 to 12 months.
Ongoing Testing: Doctors will continue regular Pap or HPV tests to ensure the cancer has not returned.
Support and Wellness:
Physical Therapy: Many patients work with pelvic floor therapists to help with comfort and strength.
Emotional Care: It’s normal to feel anxious during follow-ups. Don’t hesitate to reach out to your care team for support groups or mental health resources.

Guidance Through Your Journey
If you are facing a diagnosis or a scary test result, the process can feel overwhelming. We are here to help you navigate the next steps.
Start by asking your doctor for a clear explanation of your pathology report. Do not leave the office until you understand exactly what the results mean. If you are diagnosed with cancer, seek out a gynecologic oncologist. These are specialists who have years of extra training in cancers of the female reproductive system.
Gather your support system. Whether it is family, friends, or a professional counselor, you should not manage the emotional weight alone. Keep a notebook for your appointments to track your questions and the doctor’s answers. You are the most important member of your medical team. You have the right to ask questions, and you have the right to a second opinion.
The path forward is one step at a time. Focus on the immediate next task and let the medical experts handle the big picture. You are not just a statistic, and you are not alone in this journey. At Medfix, we are dedicated to helping you find those answers and the right specialists for your care. You don't have to walk this path alone.




Comments